Incretins Unveiled: The Hidden Keys to Vibrant Health
We discuss INCRETINS (Glucose-dependent Insulinotropic Polypeptide & Glucagon-Like Peptide-1) and how they can promote to our health and well-being. A pre-requisite to the popular Ozempic & Wegovy.
When you eat, your digestive system doesn't just break down food to get energy. It also sends out special chemical signals, called hormones, that help control how much sugar is in your blood. Two of these superheroes are GIP and GLP-1.
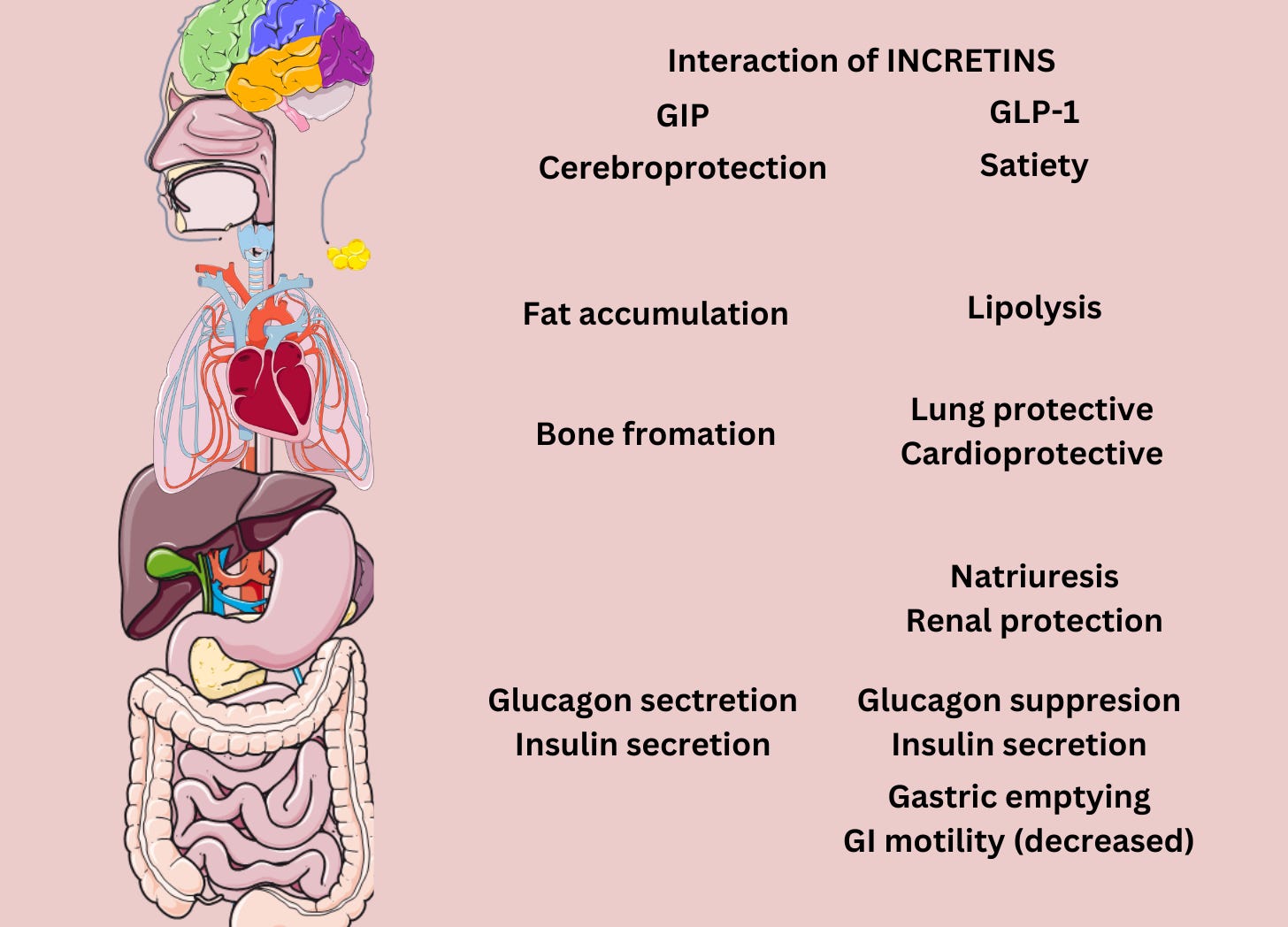
What do GIP and GLP-1 do?
GIP (Glucose-dependent Insulinotropic Polypeptide) and GLP-1 (Glucagon-Like Peptide-1) are both gastrointestinal hormones, specifically known as incretins. These hormones play crucial roles in the regulation of glucose metabolism, especially after eating.
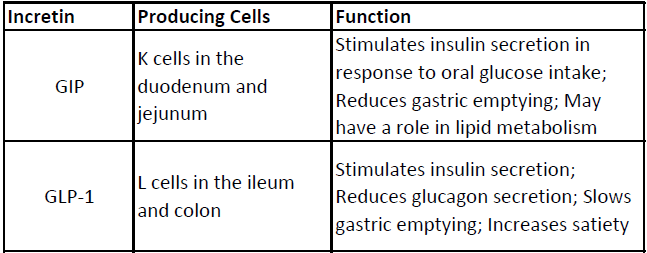
1. GIP (Glucose-dependent Insulinotropic Polypeptide):
- Produced by: K cells in the upper segment of the small intestine.
- Function: Upon ingestion of nutrients, especially carbohydrates and fats, GIP is released and works to stimulate insulin secretion from the pancreas. This ensures that glucose derived from the digestion of food is appropriately taken up by cells and used or stored, helping maintain normal blood glucose levels.
2. GLP-1 (Glucagon-Like Peptide-1):
- Produced by: L cells in the intestines, primarily in the ileum and colon.
- Function: GLP-1 is released in response to nutrient intake and has multiple effects, including:
- Stimulating insulin secretion from the pancreas in a glucose-dependent manner.
- Slowing down gastric emptying, which can reduce food intake and produce a feeling of fullness or satiety.
- Inhibiting the release of glucagon, a hormone that raises blood glucose levels.
- Offering protective effects on pancreatic beta-cells, which produce insulin.
Because of their roles in glucose homeostasis and potential effects on appetite and body weight, they have attracted significant attention in diabetes research and treatment. Specifically, GLP-1 receptor agonists are now used as therapeutic agents to treat type 2 diabetes.
Both GIP and GLP-1 come from the same area in your gut. When you eat, especially something sweet or starchy, these hormones quickly go to work. They tell your pancreas to release insulin, a helper that moves sugar from your blood into your cells. But they have some differences: GIP can also tell your pancreas to make glucagon, another hormone, while GLP-1 stops it. Glucagon does the opposite of insulin—it increases blood sugar. This balance is crucial for our health.
Incretins are a group of metabolic hormones that stimulate a decrease in blood glucose levels. They are secreted by the intestine after eating and augment the secretion of insulin released from pancreatic beta cells in response to ingested glucose.
Why are these hormones important for people with diabetes?
People with a type of diabetes called Type 2 Diabetes (or T2D) have a problem with how their body uses insulin. Recent studies have found that medicines mimicking GLP-1 can be used to treat T2D by controlling blood sugar levels and helping people lose weight.
GIP’s Special Powers
GIP has another role—it helps store energy by controlling how our body uses and stores fats. It’s like a manager telling where the energy should go. But, in people with T2D, GIP doesn't work the same way as it does in healthy people.
Exploring New Treatments
Scientists have developed medicines that act like GIP or GLP-1 to help treat T2D and weight issues. There's also a special medicine called tirzepatide that combines the powers of both GIP and GLP-1 and semaglutide that stimulates GLP-1 action. Think of it as a superhero team-up, like Batman and Superman!
Protecting our Organs
These hormones don't just control blood sugar. They also help protect our hearts, kidneys, and brains. GLP-1, for instance, can guard our heart and kidneys from disease. On the other hand, GIP helps reduce inflammation in the brain, which can be handy in battling some brain diseases.
In addition to their role in regulating insulin and glucagon, incretins also slow down gastric emptying, inhibit glucagon release, and promote satiety. The incretin system is considered a target for the treatment of type 2 diabetes, and medications that mimic or enhance incretin activity are used to manage blood glucose levels in diabetic patients.
The Future of T2D Treatment, Geroprotectives, Obesity Treatments
There's a lot of excitement around medicines that acts to increase GIP and GLP-1 activity such as Semaglutide and Tirzepatide. Semaglutide also called OZEMPIC and WEGOVY has shown excellent results in controlling blood sugar and helping people lose weight. Some experts think T2D happens because different parts of our body's system for controlling blood sugar are out of sync. The hope is that they can help get everything back in harmony. However, controversies in these medicines is also not in short supply. For example, OZEMPIC is known to have caused gastroparesis, where patients have reported severe constipation due to its inhibition of gastric motility (see image above).
Our digestive system has secret agents like GIP and GLP-1 working to keep our blood sugar levels in check. Understanding them can open new ways to treat diseases like diabetes and ensure our bodies stay healthy and happy!